On Friday June 9th, VAAP Board Member and Executive Director of Recovery Consulting, Jessica Swan, spoke at the Department of Justice in Washington, DC. The session delved into the topic of addiction science and how to reduce medication-assisted treatment (MAT) stigma in correctional settings. The presentation covered all aspects of addiction science and attendees left the session with a deeper understanding of the ways in which MAT can be used to support individuals with addiction, as well as key strategies for decreasing MAT stigma in corrections.
Jessica took some time to answer questions about the topic and her background:
How did you get involved in the area of treatment?
I originally got involved, like so many others, because of my recovery from drugs and alcohol. In 2008 I became the administrator for a drug and alcohol counseling agency, which gave me direct client contact hours and the chance to start working toward a certification in addiction counseling. I graduated college and started working in inpatient treatment in 2009, as a counselor. In 2012 I started my first nonprofit and began efforts to educate the Justice community on issues related to addiction, treatment, and recovery. I then got a master’s in criminal justice while also teaching around the country, counseling through my nonprofit, and doing research into the intersection of behavioral health and the Justice system. I also became a Master Addiction Counselor and became licensed in three states, so I could provide counseling services to more people. I specialized in family recovery from addiction and have subsequently written several curriculums and created programs for treatment centers. In 2018-2019 I became a Director for Problem-solving Courts, working in an adult mental health court, a juvenile mental health court, and a veterans treatment court. These experiences are what lead me to national research work in criminal justice and behavioral health.
What is the current state of addiction in corrections?
Not surprisingly, it isn’t good. According to the National Institute of Health (NIH, 2023), 85% of the prison population has an active substance use disorder and/or were incarcerated for a crime involving drugs or drug use. Opioid Use Disorder (OUD) specifically, according the SAMHSA, effects approximately 17 percent of people incarcerated in state prisons, and about 19 percent of those incarcerated in jails. There is a 10X increase risk of death from overdose for people with an active substance use disorder who are leaving incarceration. When compared to the general population, the risk of death from overdose increases to 40x.
Why does the stigma exist?
Society has historically viewed substance use disorders as moral problems of self will. Until recently, we have treated mental illness and substance use disorders through carved out, separate treatments or through peer-to-peer support only, rather than integrating their treatment with primary care. The medical community had not embraced the need to treat these diseases and provide appropriate referrals for services.
What does reducing stigma look like in practical terms?
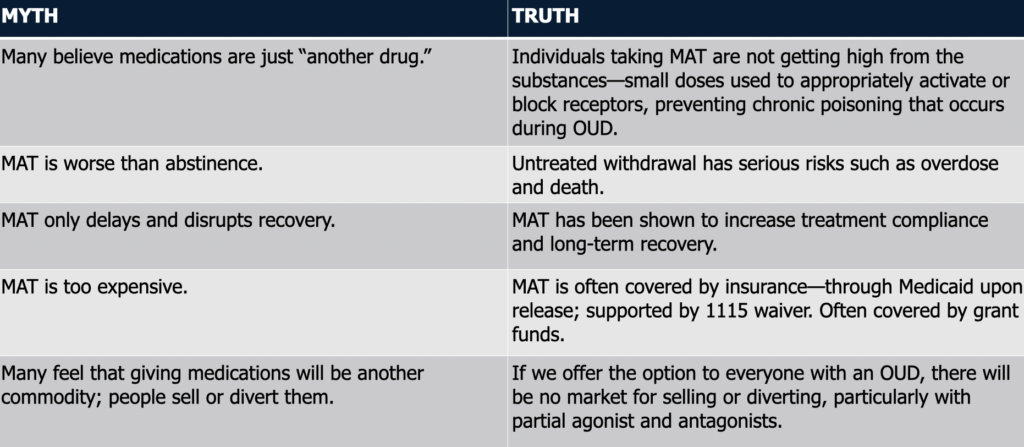
Education is the number one way to reduce stigma. Understandably, many people do not have knowledge of the brain science or the understanding of the proper treatments for these brain disorders. The more we educate people, the more we reduce stigma.
What would be the ideal outcome?
Integrated care for people with brain disorders. If we can provide services rather than punishments for people with substance use disorder (SUD), we reduce recidivism and deaths, and we improve treatment and recovery engagement. Providing integrated care for incarcerated people means screening at entry, providing MAT for all who need it, and ensuring MAT services are continued through release and re-entry into society. These are difficult tasks for the corrections community, but they are necessary, particularly since not providing these services may be a violation of civil rights and a violation of the American with Disabilities Act (ADA).
How does MAT work? (What is the process)
MAT consists of medication, counseling, and social support. It provides medication that supports the individual’s engagement in treatment services, individual and group counseling, and peer-to-peer support services. The three types of medications currently approved for treatment of SUD in corrections are methadone, buprenorphine, and naltrexone.
Why does it work (the pharmacology)?
There are three phases in the neuroprocess of addiction. The first is binge intoxication, in which the person uses an addictive substance and becomes intoxicated. This activates the person’s midbrain. Extensive amounts of dopamine (the pleasure, reward, and survival neurochemical) are released, creating a high. It also activates the endogenous opioid system, resulting in the release of large amounts of pain-relieving neurochemicals.
From there, the person goes into the second phase: The withdrawal negative affect. The extended amygdala is activated, and it causes the person to experience high levels of anxiety, irritability, and discomfort. This is from not having enough dopamine or endogenous opioid activity, due to the chronic poisoning that occurred during binge intoxication, and it results in high levels of pain and stress.
This is where medication enters into the treatment process. Medications using agonists (think “with”), partial agonists, or antagonists (think “against”), treat the dopamine and endogenous opioid systems to prevent the emotional highs and lows, the extreme pain experienced during withdrawal, and the feeling of extreme stress. Agonists work with these systems. Methadone, the agonist drug, is used in small doses and prevents the withdrawal process. Buprenorphine is a partial agonist and works in a similar way, but also includes an antagonist, so it blocks some of the dopamine and opioid receptors and prevents a high from occurring in the patient. Naltrexone is an antagonist. It works by blocking receptors and preventing craving/desire, and also the more extreme emotional highs and lows.
Do you have a specific case that you can talk about?
Yes. One case involved an incarcerated pregnant woman who we started on methadone for the safety of her and the baby. She took methadone daily while also participating in weekly group and individual counseling. Prior to her release, we connected her with a community-based provider who supplied the medication daily, all the way through the delivery of the baby and post-partum. She was able to become a responsible mother, get an apartment, land a job, and actively engage in her recovery life. It was challenging, due to the requirement that she go to a clinic to get her methadone daily, but she’s been able to stay clean for several months and for the first time in her life.
Anything else you want to add?
One big concern that sheriffs and wardens will bring up is diversion of medications in the correctional facility. There are several ways to help prevent diversion of medications from occurring. I mentioned that providing medications to anyone who needs them is the first and most effective way to reduce diversion. We also know that creating a therapeutic environment, separate housing units for MAT programs, and policies and procedures for medication distribution also help reduce diversion. Other solutions that facilities have employed include using only injectable medications – buprenorphine and naltrexone both have injectable medication options. Some facilities will crush pills prior to the client ingesting, and others have eliminated the use of strip versions of medications. That way, if any strips are found in the facility, they know that the medications have come from the outside.
Recovery Consulting is a 501c3 organization that provides specialized, confidential addiction recovery services to individuals and families. We provide support for organizations integrating mental health initiatives and facilitating leaders and staff for sustaining initiatives related to Justice and behavioral health. We offer training for legal and behavioral health professionals. We design and complete substance use disorder outcomes research, evaluation, implementation, and sustainability reporting. Whether you need counseling, consulting, training, or research support, we are here to meet your needs.

